How to prevent the elderly from falling out of bed

Falling out of bed is more common than you might think among older adults, and the consequences can be serious, such as injury, loss of confidence, or independence. In this article, we look at practical, actionable steps you can take to prevent the elderly from falling out of bed.
(This article is geared more toward fall prevention in the home setting. For care-community-specific guidance, see our posts “10 Tips for Safer Bed Exits in Long-Term Care” and “A Guide to Fall Prevention in Long-Term Care Facilities”.)
Understanding why the elderly fall from bed
Older adults may roll or fall out of bed due to a mix of health and environmental factors: muscle weakness, balance problems, certain medications, poor lighting or unstable bed setups. According to the Centers for Disease Control and Prevention (CDC), “more than one out of four older adults falls each year, but less than half tell their doctor.” Of those who fall, many will fall again. That means one bed-related fall shouldn’t be dismissed as a one-off.
To prevent future falls, it helps to understand why the fall is happening. The easiest way to do that is to look at when the fall occurs and what the person was doing just before it. The pattern often points to the underlying cause.
While the following situations are common, it is also important to speak with a healthcare professional if falls are happening repeatedly or if you notice sudden changes in balance, strength, or awareness. They can help identify medical causes and advise on the safest approach.
Is the fall happening when the person first wakes up in the morning?
Morning falls often happen when someone stands before they are fully steady, or when getting out of bed is harder because of stiffness, dizziness, or balance issues.
Is the fall happening at night during an urgent trip to the bathroom?
Night-time falls can be linked to sleepiness, low lighting, confusion on waking, or rushing because they feel the need to use the bathroom immediately.
Is the fall happening during sleep?
If someone rolls out without waking, the cause may be drifting toward the edge, reduced awareness of body position, or an unstable mattress.
Is the fall happening during transfers?
Some older adults lose balance when sitting up, turning, or standing from the edge of the bed. These transitional movements are a common risk point.
Is the fall happening on one specific side of the bed?
This can indicate that the person is using a less safe exit side, or that the room layout is guiding them toward a riskier direction.
Is the person dizzy, confused, or unsteady at the time of the fall?
This may point to medication side effects, dehydration, disrupted sleep, or changes in health.
These questions help reveal the main risk factor. For example, muscle weakness may explain difficulty with controlled movements. Medication side effects may explain dizziness. Poor lighting or clutter may explain missteps at night. A mattress with weak edges may explain drifting during sleep.
Once you understand when and why the fall is happening, you can match the right prevention steps to the cause rather than guessing. This makes the plan clearer, more targeted, and more effective.
Practical ways to prevent the elderly from falling out of bed
Bed Rails
Installing bed rails often appears to be a practical, low-cost safeguard. For as little as around $50, many households can fit hook-on or strap-on rails to an existing bed, without the need to purchase a dedicated compatible bed frame. These rails provide a clear barrier and can assist someone in turning or repositioning in bed.
However, this low-effort solution is not without risks. Between January 2003 and December 202,1 the U.S. Consumer Product Safety Commission (CPSC) reported 284 entrapment-related deaths tied to adult portable bed rails in the U.S. Although new standards have since been introduced to improve safety, the risk remains.
If you're using or considering bed rails at home, check the following carefully:
- Ensure the mattress thickness is compatible with the rail system. You must match the rail’s specifications exactly and check for any hazardous gaps between the rail, mattress, and frame.
- Verify that the rail is securely installed and locked in place; straps or retention systems should be periodically rechecked.
- Confirm the occupant can still exit safely. If the rail blocks the main exit or makes a person feel trapped, the device could increase fall risk rather than reduce it.
- Recognise the rail does not reduce the height of a potential fall, nor does it improve the surface they might land on, so a roll or climb over the rail may still lead to significant injury.
Because of these limitations, bed rails shouldn’t be treated as the full solution; they are one element of a layered fall-prevention strategy. For example, if someone regularly tries to climb out of bed, has cognitive issues, or weak balance, an adjustable low or floor-bed may be a safer, more effective investment.
Further reading: Alternatives to bed rails that actually work.
Low and floor-level hospital beds
Lowering the bed is one of the most effective ways to reduce harm if someone falls out of bed. The logic is simple: the lower the bed, the shorter the fall, and the less force on impact.
This is backed by research. In an analysis by Dr. George Zaphir, lower bed heights were shown to significantly reduce injury risk, with low beds producing up to 40% less impact force compared to standard beds.
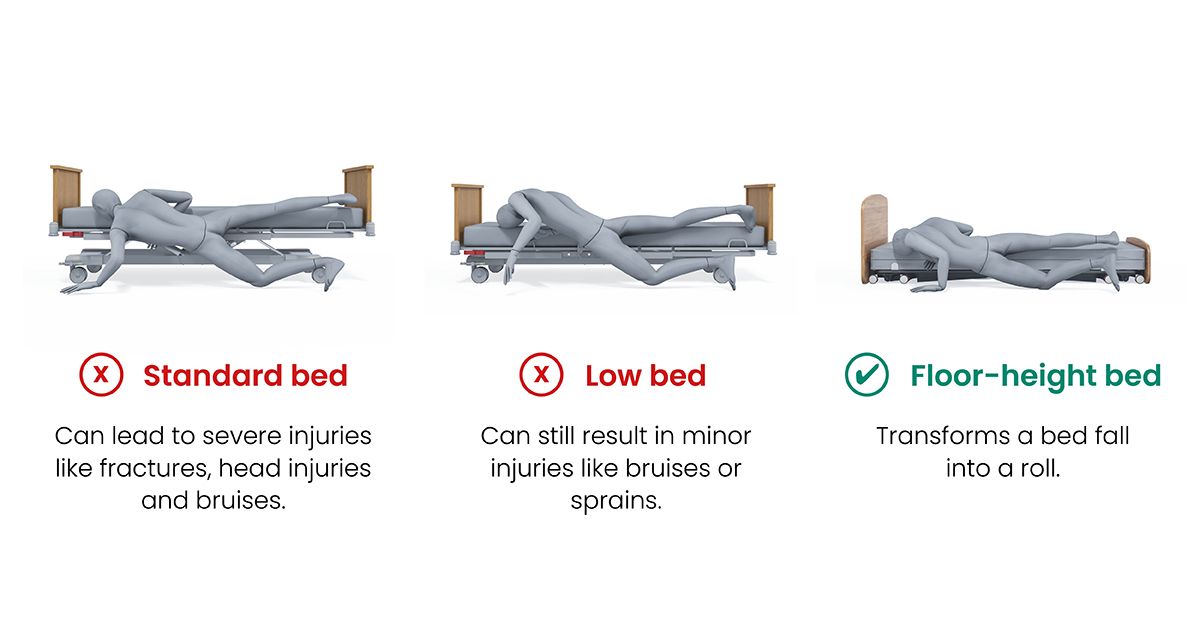
Building on this principle, the Contesa® FloorBed lowers all the way down to floor level. This design helps in two ways:
- Less distance to fall
If someone accidentally rolls out of bed, the drop is very small. This greatly reduces and, in most cases, eliminates the chance of injury. - Early self-correction
When the bed is at floor-level, people often feel the floor with a hand or foot before they fall fully out. This small feedback moment often makes them readjust and stay safely on the mattress.
The Contesa also raises to a safe working height, so caregivers or family members can help with transfers or morning/evening care. This means you get a very low bed for safety at night, and a comfortable height during the day, without compromising either.
For extra protection, you can place a safety mat next to the FloorBed. This creates a cushioned landing area and turns any fall into more of a gentle roll, adding another layer of protection.

Cost considerations
Low beds and floor beds tend to fall into the mid-premium price range. They cost more than standard home beds, but when you compare that to the potential cost of a single fall, emergency care, hospital treatment, lost mobility, many families find the investment worthwhile.
Further reading: How Much Does a Hospital Bed Cost?
Mattresses that support fall prevention
Once the bed height is managed, the mattress becomes the next line of defence. A mattress that is too soft or sinks at the edges can make it easier for someone to slide, tilt, or roll toward the side. A mattress with firm edges or built-in bolsters creates a more stable boundary. This helps in several ways:
- The edge doesn’t “collapse” when someone sits or lies near it.
- The person can feel where the edge is, which helps prevent drifting off the side during sleep.
- Transfers are safer because the edge gives a more solid platform when someone sits up to stand.
Some mattresses also come with raised sides, which help prevent rolling off the mattress and can reduce the risk of entrapment between the mattress and bed rails when rails are used.
Room Layout
The way the room is set up around the bed has a big impact on fall risk. Often, falls do not happen in the middle of the bed, but when someone is trying to move into or out of it.
Dr Patricia Quigley, a fall-prevention expert talks about “using the wall” and thinking carefully about bed position and exit paths in her “10 tips for safer bed exits” article.
Whilst the article is directed at care communities, for a home bedroom, you can apply the same thinking:
- Create a “safe side” for exits
• If possible, place one side of the bed against a wall. This reduces the number of open sides someone can accidentally roll off.
• Make the other side the “planned exit” side, with clear space and any supports (such as a grab handle or pole) on that side. - Keep the floor clear
• Remove loose rugs, trailing cables, storage boxes and other clutter from beside the bed. Home safety resources and fall-prevention guides consistently list clutter and loose rugs as common causes of trips and falls in older adults.
• Make sure there is enough space to stand up and turn without bumping into furniture. - Think about where the person is actually moving
• Look at the real route they take at night: bed to bathroom, or bed to a chair or commode.
• Make sure they do not have to weave around furniture or step over objects. A “straight, simple path” is usually safest.
Consider Lighting
Nighttime and early-morning hours can be higher-risk periods for older adults. People often wake up feeling sleepy or disoriented, and visibility is naturally lower. Poor lighting makes it harder to judge distances, notice objects on the floor, or steady themselves when getting in or out of bed.
The right lighting doesn’t need to be bright; what helps most is low-level, gentle lighting that turns on when needed and makes the path around the bed easier to see.
Practical options include:
- Plug-in night lights in the bedroom or hallway. These provide a soft glow that reduces tripping hazards without waking the person fully.
- Motion-sensor lights that switch on automatically when someone gets out of bed or walks past. These remove the need to search for a switch in the dark and can help build confidence during night-time bathroom trips.
- Guiding night lights placed near the bed. A small study found that this type of gentle, directional lighting reduced fear of falling and improved sleep quality in older adults.
Top tips
- Place at least one low-level light within reach of the bed or along the route to the bathroom.
- Keep lighting soft and even, avoiding harsh glare or deep shadows.
- Avoid leaving the room in total darkness, especially if the person wakes frequently at night.
Supporting precautions
Finally, there are several simple devices that can add extra layers of protection around the bed. None of these on their own is “the answer”, but combined with a low bed, a good mattress, and a safe room layout, they can help reduce risk further.
- Grab bars placed on or next to the bed can give the person something solid to hold when standing up, turning, or lowering themselves back down. The Contesa FloorBed has an optional folding assist bar that can support transfers and repositioning and simply folds away when not in use.
- Bed-exit alarms use a sensor on the mattress or a small mat on the floor beside the bed. When the person gets up, an alert sounds in the home, so a caregiver knows they may need help.
- A fall mat is a thick, padded mat placed on the floor next to the bed. It is particularly useful alongside a low or floor-bed. Accora FloorBeds have an optional high-safety mat. The mat is the same height as the bed with a 6" mattress, turning a fall into a roll onto the safety mat.
Putting it together, the idea is not to rely on one device or one change, but to combine a few well-chosen steps:
- A low bed or floor-level bed to reduce height.
- A mattress with firm edges to keep the person stable and make transfers easier.
- A sensible room layout with a safe exit side and clear floors.
- Gentle lighting at night so they can see where they are going.
- Extra supports like assist bars, alarms, wedges, and floor mats where needed.
Quick Home Bed-Safety Checklist
Use this checklist to assess your loved-one’s bed and bedroom environment:
- Is the bed height safe (e.g., person can place feet flat and get up without over-stretching)?
- Is the mattress stable, edge-supported, with no major gap between mattress and frame?
- Is there minimal clutter beside the bed, and good lighting for night‐time?
- Are there any bed safety rails or cushioned mats appropriate to the person’s mobility?
- Is their strength/balance been reviewed in the last year? Have medications, hearing and vision been checked?
Make one change this week, for example, secure or remove one loose rug, install a night light or test the bed height.
A safer bedroom helps, but daily habits matter too
A safer bed and bedroom reduce risk, but the environment is only one part of the picture. A person’s strength, balance, medications and routines also influence how likely a fall is.
Staying Active: Strength, Balance and Movement
Lower body weakness is one of the strongest predictors of falls. The CDC identifies strength and balance as key areas for prevention. Regular movement helps maintain coordination. Short walks, chair-based exercises and light strength work can be enough to help elderly people stay steadier on their feet.
Reviewing Medications, Vision and Hearing
Some medications cause dizziness, drowsiness or slower reaction times. These should be reviewed regularly with a clinician. Vision and hearing also influence balance and awareness. Routine checks help catch changes early and reduce fall risk.
Bringing it all together
Preventing falls from bed at home often requires a combination of small changes rather than one single fix. Lowering the bed, choosing the right mattress, planning a safe room layout and using good lighting create a safer environment. Supporting strength, reviewing medications and helping with night-time routines complement these physical changes.
Together, these steps can significantly reduce the likelihood of a fall and help older adults feel safer, more confident and more independent.
FAQs
What does it mean when an elderly person keeps falling?
Frequent falls often indicate that something has changed in the person’s health, strength, balance or environment. Common causes include medication side effects, poor lighting, muscle weakness, dizziness, or vision changes. Repeated falls are never “normal ageing” and should be discussed with a healthcare professional to rule out underlying medical issues.
What should I do when the elderly keep falling?
Start by noting when the fall happens and what the person was doing just before it. This helps identify the cause. Remove hazards such as loose rugs or clutter, improve lighting, review medications with a clinician. If falls continue, contact a healthcare professional for further assessment.
How do you prevent the elderly from falling out of bed?
Prevention usually involves a combination of steps. Lowering the bed reduces the height of a fall. A mattress with firm or raised edges helps keep the person centred during sleep. Bed positioning, night-time lighting, and a clear exit path reduce risk when getting up. For some elderly people, using a floor-level bed or a fall mat beside the bed offers extra protection.
Take a look at Accora's floor-level hospital beds
How to keep an elderly person from getting out of bed at night?
It's important to note that you can't stop a person getting out of bed at night but you can take steps to encourage less nighttime movement. If the person gets up because they need the bathroom, a bedside commode or motion-activated night light can reduce rushing. If confusion or nighttime wandering is the issue, speak with a healthcare professional, as this may signal changes in health or medication effects. Ensuring the bed is at a safe height, simplifying the room layout and placing essential items within reach can also reduce unnecessary night-time movement.
.png)


