Identifying and treating unstageable pressure ulcers

While all pressure ulcers significantly impact a patient’s quality of life and outcome, unstageable pressure ulcers pose particular challenges. They can be painful and dangerous, and they obscure the full extent of underlying tissue damage.
Because unstageable ulcers are so challenging to treat, many patients live with them for years.
"The goal is to prevent pressure injury as much as we can, but when they do occur, it's crucial that rehab is part of the healing process with the interdisciplinary team," says Patricia Larkin-Upton, DPT, a physical therapist at PowerBack Rehabilitation, who’s board-certified in skin and wound management.
Larkin-Upton has seen countless patients’ lives improve when their difficult skin trauma finally heals. For example, one patient she treated endured a painful amputation wound for three years that continuously drained and emitted an odor. It was so severe that he became isolated from friends, family and his community.
The patient finally received intensive, interdisciplinary care at a skilled nursing facility and the wound healed over a few months. "He cried when that wound closed, and he was able to go home. It changed his whole life," she says.
The patient regained independence, reconnected with his community and resumed everyday activities such as driving and going out.
What’s an unstageable pressure ulcer?
An unstageable pressure ulcer typically occurs in people who are immobile for extended periods, along with other comorbidities. The wound is covered by necrotic tissue such as eschar or slough, which obscures the wound's depth and underlying tissues. "An unstageable wound typically goes deeper than it initially appears, and removing the dead tissue often reveals a significantly more severe injury," says Larkin-Upton.
This makes unstageable ulcers particularly challenging, as proper treatment decisions and interventions depend on accurate staging of wound severity.
Identifying an unstageable pressure ulcer
Proper pressure ulcer identification requires careful examination for extensive necrotic tissue. The wound's true severity is likely hidden beneath the surface.
Key indicators of an unstageable pressure ulcer include:
- Extensive necrotic tissue (eschar or slough)
- Inability to visualize underlying structures clearly
- Potentially deeper than initially assessed
"We should not stage a wound without seeing the base because removal of necrotic tissue can reveal a wound deeper than expected," says Larkin-Upton.
Common complications
Unstageable pressure ulcers are painful and can lead to numerous complications, including infections like cellulitis, osteomyelitis or even sepsis.
They often become chronic wounds, which significantly impair mobility and increase fall risks –– particularly among frail or elderly patients.
"Falls can increase due to impaired sensation or frailty in patients with these severe wounds," says Larkin-Upton.
Treatment strategies
Addressing unstageable ulcers requires a coordinated, multidisciplinary approach. Treatment usually begins with debridement –– removing necrotic tissue — to reveal the wound base and stage the ulcer accurately. Surgical, enzymatic, autolytic and biological methods, such as sterile maggot therapy, are standard options.
Choosing the right dressing is also critical:
- Alginate dressings: High exudate management
- Hydrogel dressings: Autolytic debridement facilitation
- Antimicrobial dressings: Prevent and manage infection
Emerging adjunctive treatments, including negative-pressure wound therapy (NPWT), infrared therapy and electromagnetic therapy, offer promising results. "These external modalities help increase circulation and nutrients to the wound," says Larkin-Upton.
Patient education for prevention
Some basic patient and caregiver education, such as teaching people how to check skin and identify issues early, can help prevent unstageable ulcer wounds. “People who live alone or who don't have knowledge about the risk of deep wounds, aren't checking their skin and often have multiple comorbidities. By the time they get to us, there's been some significant tissue damage,” says Larkin-Upton.
Education should focus on the following:
- Regular skin inspections by patients or caregivers
- Moisture control and maintaining cleanliness
- Awareness of medical conditions that increase risk, such as diabetes or neurological disorders
- Medication reviews to reduce risk factors
- Nutritional management for overall health and wound healing
Introducing interventions early like repositioning the patient and offloading high-risk areas (like any bony prominent area) can help prevent unstageable pressure ulcers.
"Prevention is key. Addressing risk factors early significantly reduces the likelihood of developing severe wounds,” says Larkin-Upton.
Fall prevention, together with wound management
Patients with severe wounds often have heightened fall risks due to decreased mobility, pain or medication side effects. “It’s critical to implement fall prevention measures alongside wound treatment,” says Larkin-Upton.
Who’s at high risk?
Knowing who’s at high risk of developing skin trauma can help prevent it. Comorbidities like cardiovascular disease, pulmonary disease, neurological comorbidities, spinal cord injuries and diabetes all put people at a higher risk because their blood flow, sensation or immune responses are slower.
A history of skin breakdown, incontinence or excess moisture put patients at more risk for recurrence. Low vision or cognitive deficits can also keep people from checking their skin as easily and cause breakdown. Even sleeping aids that can cause people to be more immobile can increase the risk.
Unfortunately, skin breakdown can also be an inevitable sign of someone who’s nearing the end of life. “The skin is an organ, so when it starts to fail you'll often see it's a result of other internal organ failure happening, like the renal system or cardiovascular system shutting down,” says Larkin-Upton.
Technology to prevent pressure wounds
Technology to help identify and treat pressure wounds is increasing.
Pressure-prevention beds and chairs
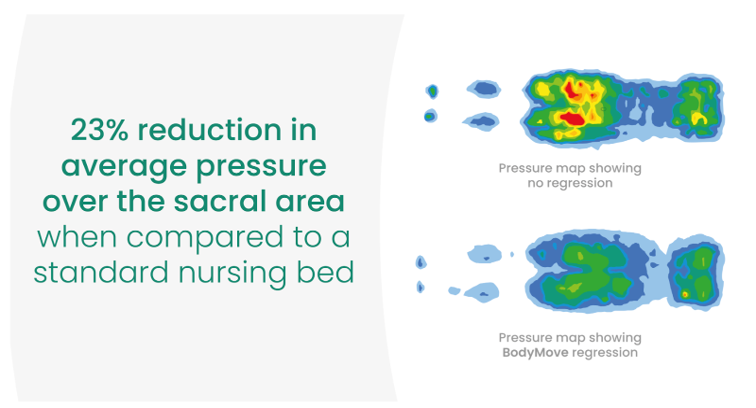
Conventional non-regression nursing beds can increase pressure loading due to the compressed nature of the body in an upright, seated position. Instead of compressing the sacral area as other profiling beds do, the Empresa FloorBed creates more surface space by moving the mechanisms of the leg rest toward the foot of the bed and the backrest toward the head of the bed as it rises.
Accora’s Configura chairs come with a high-risk pressure prevention cushion built in as standard. This will provide enough prevention for some users. For very high-risk users, the cushion can be easily removed and replaced with a more appropriate cushion for that service user.
Temperature gauging
New technology devices and even fabric-based wearable sensors can sense skin temperature changes at a more sensitive level than human hands.
Pressure mapping
New technology that senses the pressure on an area can help patients and caregivers identify what positions and beds work best.
“There's a lot of neat new technology coming out that can help people identify areas of risk or areas that have micro damage before true damage occurs,” says Larkin-Upton.
Interdisciplinary team approach
Healing complex wounds requires collaboration from medical professionals, therapists, dieticians, social workers, caregivers and patients themselves. "A team-based approach provides the strongest support system for effective healing," says Larkin-Upton.
Together, a team of clinicians and caregivers can prevent and mitigate unstageable pressure ulcers through early recognition and strategic management. While some wounds may not fully heal, the focus remains on patient comfort, preventing complications and improving quality of life.
"Our goal may change based on the patient's medical condition, and the patient and family goals. Comfort and infection prevention are sometimes the most crucial interventions," says Larkin-Upton.
Stay updated with our fall prevention content and learn about our free online training sessions by signing up for the Accora Cares newsletter. We tackle challenges senior care facilities face, including fall prevention, pressure ulcer management and compliance.
References
Image: Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. NPUAP, EPUAP, and PPPIA, 2014.
%20lower.png)








